Total Parenteral Nutrition (TPN) and Enteral Nutrition
A total parenteral nutrition (TPN) is a way of delivering nutrition to the body through the veins. It literally bypasses the gastrointestinal tract. The dripping solution is introduced directly into the vein, which is beneficial to patients who cannot be fed by mouth. (1, 2)

Image 1: A solution used for total parenteral nutrition.
Picture Source: www.enasco.com

Picture 2: A female patient who has a total parenteral nutrition line.
Photo Source: 78.media.tumblr.com

Photo 3: A total parenteral nutrition can also be given to children.
Image Source: netdna-ssl.com
Total parenteral nutrition indications
It should be given to people who cannot get the nutrition needed by the body through eating such as in the case of:
- Intestinal obstruction
- The small intestine has problems absorbing nutrients properly
- Gastrointestinal fistula/abnormal connection
- The bowel needs to rest for a while such as in the case of pancreatitis, Crohn’s disease, and ulcerative colitis.
- Severe burns
- Severely malnourished person
- Multiple fractures
- Individuals who are to undergo major surgery, radiation treatment, and chemotherapy
- Acquired immune deficiency syndrome (AIDS)
- Sepsis (widespread infection) (1, 2, 3, 4)
Total parenteral nutrition procedure
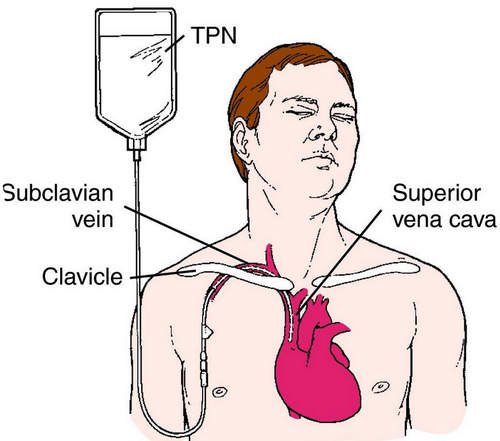
Image 4: A cartographic image of the total parenteral nutrition site.
Picture Source: www.infusionsolutionsinc.com
Total parenteral nutrition is introduced to the body through the large central vein. A sterile catheter is inserted into the vein located in the chest under a local anesthesia. After a successful placement of the catheter, a chest x-ray is performed to see to it that the placement is correct. The procedure of inserting catheter for TPN is usually performed in the hospital setting. However, there are instances when the procedure is performed in the home setting but with the supervision of a private nurse or experienced caregiver. (3, 4, 5)
Total parenteral nutrition guidelines
The content of TPN is mixed on a day to day basis to make sure that everything is fresh and sterile. The content of the TPN solution is determined based on the patient’s age, height and weight, and medical condition. A TPN solution contains:
- Sugar (dextrose)
- Protein (amino acid)
- Fats (lipids)
- Electrolytes like sodium, potassium, magnesium, calcium, phosphate, zinc, manganese, copper, chromium, and chloride
- Vitamins
- Insulin (5, 6)
What to keep in mind?
An adult patient would need about two liters of TPN solution on a day to day basis. Although the exact amount varies depending on the patient’s overall health condition. While the patient is on TPN, his weight should be thoroughly monitored including health parameters like the urine output, blood count, and blood sugar level.
The condition of the liver and kidneys should be monitored too. Ideally, TPN should be given to the patient for a short period of time. Once the patient is allowed to eat through the mouth, the catheter should be removed right away. (5, 6, 7)
Total parenteral nutrition complications
- Mechanical complications pertain to the manner the central venous catheter is inserted in the veins. If there is problem in the placement of the catheter, there is a possibility that the patient could suffer from pneumothorax, cardiac arrhythmia, and brachial plexus.
- Venous thrombosis is one of the TPN complications that could lead to death. Signs and symptoms of venous thrombosis include neck vein distention, swelling of the face, as well as ipsilateral arm. The possibility of venous thrombosis is high in people with malignancy, dehydration, sepsis, and venous stasis. (5, 7, 8)
- There is also a greater risk for infection. The harmful microorganisms can grow in areas where the catheter is inserted such as the catheter tip. It is important to strictly adhere to the safety measures and aseptic procedure so as to prevent infection.
- Metabolic complications can arise too. It can arise in the beginning of the feeding or at the end of the feeling. Metabolic complications can be avoided by a strict monitoring and adjusting the intake based on the patient’s response to TPN. As with the late metabolic complications, they could be caused by pre-existing abnormalities and failure to monitor the feeding process. Hence, it is of utmost importance to thoroughly monitor the patient while on total parenteral nutrition to notice any abnormalities the soonest time possible.
- There is also a risk for fluid and electrolyte imbalance. Managing the level of electrolyte is quite difficult, especially if the patient is in total parenteral nutrition. Most of the time, the level of electrolyte is outside the normal range and the TPN alone is not the one responsible for it. The primary reason is the patient’s underlying medical condition. To somehow keep the level of electrolyte within the normal range, you need to make an incremental dose adjustment while the root cause of electrolyte imbalance is addressed.
- There is a possibility of refeeding syndrome, which is common in severely malnourished patients. These patients have a severely low level of minerals such as phosphate, magnesium, and potassium. In the case of refeeding syndrome, there is a possibility that various organs of the body will be affected, especially the heart. If not addressed properly, it could lead to paralysis, cardiac dysrhythmias, acute respiratory failure, liver dysfunction, nephropathy, and heart failure. (5, 8, 9, 10)
What is the difference between Enteral and Parenteral nutrition?
Many are confused between enteral and parenteral nutrition. They thought that the two are the same, but they are not. What is enteral nutrition? It is a feeding method that uses the gastrointestinal tract to deliver nutrients to the body. It can be in the form of liquid supplements or the usual oral diet. In other words, an enteral nutrition is a tube feeding.
On the other hand, parenteral nutrition pertains to the delivery of nutrients through the vein and is given to the patient who has a problem in their gastrointestinal systems such as short bowel syndrome, bowel obstruction, ulcerative colitis, and the likes. Both deliver nutrients to the body but the route is different. The solution is also different. The parenteral nutrition route is more complicated than the enteral nutrition. (2, 5, 8)
| Differences | Enteral | Parenteral |
| route | Gastrointestinal Tract | Large central vein (venous route) |
| tool | tube | catheter |
| types | Tube feeding/sip feeding/gastronomy/tube insertion | Central and peripheral |
| calories | 1-2 kilo calorie/ml | 25 to 30 kilo calories per kg per day |
| indications | patient cannot take anything by mouth for five to seven days | only indicated if enteral feeding is not possible |
| Nutritional solution | usual oral diet/liquid supplement | A mixture of different nutritional requirements of the body such as vitamins, minerals, fats, protein, and sugar. |
References:
- https://en.wikipedia.org/wiki/Parenteral_nutrition
- https://www.msdmanuals.com/professional/nutritional-disorders/nutritional-support/total-parenteral-nutrition-tpn
- https://www.g-pact.org/gastroparesis/nutrition/intravenous-nutrition/tpn
- http://www.nutritioncare.org/about_clinical_nutrition/what_is_parenteral_nutrition/
- https://medlineplus.gov/ency/article/007239.htm
- https://www.inmo.ie/article/printarticle/4377
- https://healthosphere.com/total-parenteral-nutrition/
- https://lifeinthefastlane.com/ccc/total-parenteral-nutrition-tpn/
- https://www.healthline.com/health/parenteral-nutrition
- https://www.oncologynurseadvisor.com/palliative-care/benefits-and-risks-of-parenteral-nutrition-in-patients-with-cancer/article/209090/