Fatty Liver
What is Fatty liver?
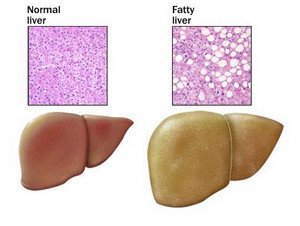
Fatty liver is a condition where fat in the liver exceeds beyond 5-10% of the weight of the liver [1]. Fat in the liver accumulates in the form of large vacuoles of triglycerides through steatosis (i.e. abnormal lipid retention within a cell) [2].
Otherwise known as fatty liver disease (FLD), it is classified as either alcoholic or non-alcoholic liver disease, depending on its cause. FLD is often times benign, however, accumulation of simple fat in the liver leads to greater risks that may cause further damage such as inflammation (steatohepatitis) and scarring of the liver [4].
Fatty liver disease can often be reversed through a change in lifestyle [3].
picture:normal vs fatty liver
Source: Mayo Foundation
How does the liver become fat?
One of the functions of the liver is to filter fats. The liver is clogged when too much fat accumulates on the spaces surrounding liver cells (hepatocytes). This then causes the liver to enlarge and become heavier, thus it is termed a fatty liver.
This condition reduces the liver’s function which is to filter toxins and other harmful substances from the blood, which further aggravates the work of the liver to metabolize fats [5].
Signs and Symptoms
Fatty liver disease often doesn’t show any outward symptoms, and sometimes only known when patients undergo medical tests [3]. When the disease advances, which may take years or even decades in the making [1], that’s where various symptoms begin to show. Symptoms such as:
- Fatigue
- Weight loss
- Abdominal discomfort
- Vomiting blood
- Pain in the centre or upper right of abdomen (due to enlargement of liver pressing to other organs)
- Weakness
- Nausea
- Confusion or difficulty concentrating
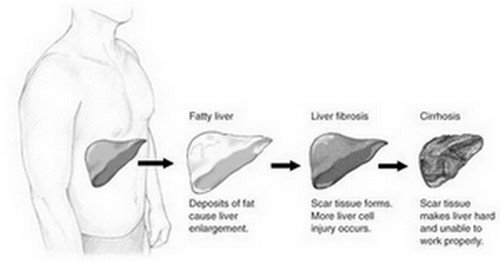
When the disease is caused by alcoholic means, symptoms worsen when heavy drinking is continued. When it is non-alcoholic, the disease may easily be reversed, but may also become worse, depending on its cause (i.e. genetic). Cirrhosis may develop either way [1], wherein the liver begins to lose its function when liver cells are replaced by scar tissue due to enlargement for which you may have the following symptoms:
- Jaundice or yellow discoloration of the skin, eyes, and the mucus membranes
- Bruising and bleeding caused by decrease of coagulation factors produced by the liver
- Liver failure
- Fluid retention
What causes fatty liver?
Fatty liver has multiple causes but the leading cause worldwide is excessive alcohol intake and obesity. It is also associated with metabolic syndrome (diabetes, hypertension, high levels of triglycerides, insulin resistance).
The people who have higher risk of this disease are those who are middle-aged and overweight, obese, suffer from diabetes and hypertension. However, some people may not have these factors but still develop fatty liver disease.
There are some nutritional causes of fatty liver, such as:
- Starvation and malnutrition,
- Rapid weight loss,
- Long term use of parenteral nutrition (direct infusion of nutrients in the blood stream); and
- Intestinal bypass surgery for obesity [4].
If the cause is considered in light of alcohol, the disease may be alcoholic or non-alcoholic.
Alcoholic Fatty Liver disease
People who drink excessive alcohol have 90-100% chance of having a fatty liver [1]. Heredity may also be a factor of this disease because sometimes, alcoholism is passed down to offspring and also, genes that may affect the metabolism or breakdown of alcohol. The development of alcoholic liver disease is commonly influenced by hepatitis C, obesity, diet, and overload of iron.
Non-Alcoholic Fatty Liver Disease
Fatty liver disease that develop in people who drink no alcohol or minimal alcohol have higher risk of developing non-alcoholic steohepatitis (NASH), wherein the fatty liver has inflammation. A simple fatty liver is usually benign, but when NASH develops, serious conditions may occur for it may lead to permanent liver damage. 20% of adults with NASH develop cirrhosis (liver scarring) and 11% may experience liver-related deaths [4].
NASH is usually caused by different medications that affect the liver, viral hepatitis, inherited liver disease, rapid weight loss and malnutrition [1]. Recent studies suggest that over accumulation of bacteria in the small intestine may cause non-alcoholic fatty liver disease [1].
Non alcoholic fatty liver disease may progress in the following stages:
- Simple steatosis (fatty liver),
- NASH (steatosis with inflammation),
- Liver cirrhosis (steatosis with liver hardening and liver scarring),
- Complete liver failure or in some cases, liver cancer and then
- Death unless liver transplantation is performed.[5]
picture:progression from fatty liver to cirrhosis
Source: news-medical.net
Fatty liver in Children
Fatty liver disease in children occurs more now than before due largely to childhood obesity. It affects 22-53% of obese children [2]. Children as young as four years of age may have fatty liver disease [2].
How is fatty liver diagnosed?
Since fatty liver is often a silent disease, certain tests such as blood tests, imaging tests and liver biopsy are needed to ascertain diagnosis after a routine check up that includes health history and physical examination.
- Blood tests may show elevations of certain liver enzymes such as alanine aminotranferase (ALT) or aspartate aminotransferase (AST)
- Abdominal ultrasound may show an obvious fatty liver.
- Liver biopsy is usually done to examine the condition of liver cells, if inflammation has occurred and if fat content is beyond normal [1]. The doctor will insert a needle in the liver and obtain a sample tissue which will be examined under the microscope.
Treatment for fatty liver disease
Currently, there is no exact medication to treat fatty liver disease. It is usually treated through treating its underlying causes such as obesity and diabetes [2]. Certain clinical tests are underway to find medication that decrease fat in the liver. What we can do now is to improve the condition by sticking to a treatment regimen.
- Losing weight can help loosen the fat in the liver. Losing weight must be gradual, so you must stir away from extreme gastric bypass surgeries and starvation diets. Losing not more than 1 to 2 pounds a week is recommended [5].
- Keep a balanced diet and be active. Exercise at least 30 minutes a day and avoid consuming rapidly digested carbohydrates such as rice, bread, potatoes, sports drink and juice which have concentrated sugar [1].
- Avoid triglycerides or fatty diets. Limit fat consumption to less than 30% of daily caloric intake [5]
- Avoid unnecessary medications that may worsen your disease [1]
- See your doctor regularly for regular check-ups. Gastroenterologist is preferred [3].
- Avoid alcohol even if what you have is non-alcoholic fatty liver disease.
- Help your liver by treating underlying disease like type II diabetes and hypertension.
- Fatty liver disease caused by bacteria can be treated by taking probiotics, dietary supplements containing good and live bacteria [1].
- Antioxidants and certain vitamins (silymarin, vitamin C, vitamin E, pioglitazone, melformin) may help [1, 5].
- If you are already overweight, don’t wait around and prevent developing the disease because you have a higher risk of developing a fatty liver. Be proactive, exercise and have a balanced diet, before everything may be too late.
References:
- www.webmd.com
- www.news-medical.net
- www.betterhealth.vic.gov.au
- www.liver.ca/liver-disease
- bestfattyliverdiet.com
Leave a Reply
You must be logged in to post a comment.