Swollen Ear lobe
Swollen ear love is the enlargement and inflammation of the earlobe. There are many reasons why the earlobe gets swollen.
The severity of the condition depends on the root cause of the problem. Sometimes the swelling can affect a particular area of the earlobe, but most of the time it can affect the entire earlobe. (1, 2)
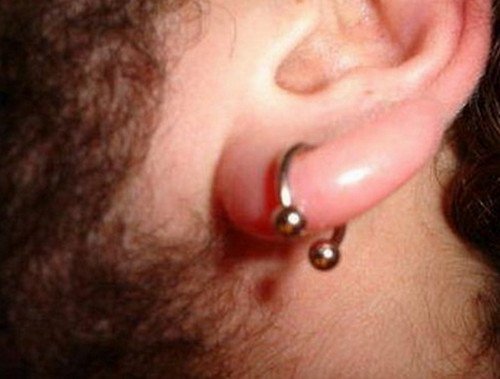
Image 1: A person with a swollen ear lobe secondary to piercing infection.
Picture Source: www.healcure.org

Photo 2: Swollen earlobe secondary to mastoiditis
Picture Source: img.tfd.com

Image 3: Ear infection leading to swelling of the ear lobe and other parts of the ears
Photo Source: www.healthyhowto.org
What are the clinical manifestations?
- Rash
- Pain and tenderness
- Crusting and flaking
- Itching
- Lumpy or bumpy feeling when you touch the earlobe (2)
Swollen Ear Lobes Causes
- Earlobe piercing – If you have a piercing, there is a tendency that your earlobe will swell, especially right after the piercing procedure. The swelling and pain could last for a few days. However, if the inflammation, swelling, and pain go on for a long period of time, then it could suggest a possible piercing infection.
- Allergy – If you have sensitive skin, then you are prone to allergic reaction. Hair sprays, earlobe piercing jewelry, shampoo, or soap can all cause allergy. Fashion earrings usually have nickel, which can cause itching and swelling for people with sensitive skin. If you know that your skin is prone to allergy, you have to be extremely careful when it comes to using skin care products and jewelry. (4)
- Mastoiditis – It is the infection of the mastoid bone, which is located behind the ear. It causes fever, pain, redness, and swollen earlobe.
- Insect bite – If your earlobe is itchy, swollen, and reddened, it could be possibly cause by insect bites. Swollen earlobe secondary to insect bite does not last. It usually takes a few hours for the pain and inflammation to subside. (3)
- Abscess in the earlobe – An abscess is a painful collection of pus secondary to bacterial infection. If you have abscess ear lobe, you should seek medical attention right away. It usually takes antibiotics and draining to thoroughly get rid of the abscess, although most abscess naturally drain, shrink, and dry away.
- Swollen earlobe secondary to pimple – A pimple in the earlobe area can cause swelling and pain. It can also cause redness and tenderness. It usually goes on its own, but if it is bothering you, then you should use over the counter products for pimples. Just make sure that the product won’t get inside your ear.
- Cauliflower ear – A cauliflower ear or medically known as hematoma auris is a deformity of the ear secondary to trauma or injury. If the condition is not treated, it can affect the proper circulation of blood. It could lead to swollen ear lobe with lump. In severe cases, a cauliflower ear can cause scar tissue formation. It causes deformed ear appearance. (5)
- Cyst and boils in the earlobe – Swollen outer ear lobe can be caused by cyst or boil. A cyst looks like a blister and can occur in any parts of the body. Various factors could lead to the formation of cyst such as infection, cell defects, trauma, blocked ducts, parasites, tumor, and so on. If the swelling of ear lobe is caused by cyst, then it should be drained or surgically removed. On the other hand, a boil is a red and painful lump secondary to infection. It is usually caused by Staphylococcus bacteria.
- Cellulitis – It is an infection of the deep layer of the skin as well as the underlying tissues. If the infection is severe to the point that it affects your day to day living, then you need to seek medical help. The doctor will thoroughly assess the condition of your earlobe and will prescribe the right medication and course of treatment. (5, 6)
- Otitis externa – A medical condition caused by inflammation of the external ear canal. It is tagged as swimmer’s ear because exposure to water makes the ear susceptible to infection. If you are experiencing swollen ear lobe infection like this, then you need to see your doctor right away. Not seeking medical help could lead to hearing loss.
- Ear cancer – A cancer can appear in any parts of the body. A few types of cancer can cause swollen ear lobe and lymph nodes. If the lymph node is involved, it could suggest that you are possibly suffering from lymphoma.
- Other causes of swollen ear lobe – Other factors that could lead to swelling of the ear lobe include contact dermatitis, folliculitis, rash, or secondary to surgical operations.
Earlobe Infection Treatment
How to treat swollen ear lobe? There are many ways to treat an earlobe infection. To effectively treat a swollen earlobe, the root cause of the problem should be first established. If it is caused by bacterial infection, then an antibiotic treatment should be started.
If it is caused by allergy, the symptoms are best managed using antihistamines. For pimples and cyst, draining and surgical removal are the best remedies. (6, 7)
How to treat swollen earlobe at home?
- Cold compress – To alleviate swelling, the blood flow on the area should be decreased. Cold compress helps decrease the flow of blood thereby alleviating pain and discomfort. Make sure that when you apply cold compress, you do not leave it on your skin for a long period of time.
- Warm compress – If the swelling of the earlobe is caused by sebaceous cyst, a warm compress can help alleviate the symptoms. It relieves pain and promotes proper blood circulation.
- Sal water solution – How does salt water solution help in alleviating swollen ear lobe? It works by dehydrating the cells thereby reducing swelling. To create your very own salt water solution, you should dissolve ¼ teaspoon of sea salt to 8 ounces of distilled water. You can also use tap water. Get a clean cotton ball and soak in the salt water solution. Place the cotton ball on the swollen ear lobe for a few minutes. Do this at least three times a day until the swelling subsides.
- If the swelling does not go away despite desperate measures, the best thing to do is to consult your doctor. (7, 8, 9, 10)
References:
- www.wowremedies.com
- www.healcure.org
- www.healthedition.org
- www.medhealthdaily.com
- www.wisegeek.com
- www.healthyhowto.org
- www.rightdiagnosis.com
- www.healthline.com
- www.medbroadcast.com
- www.wisegeek.org

 Image 1: An image of a child with Sotos syndrome with prominently large head circumference and wide set eyes.
Image 1: An image of a child with Sotos syndrome with prominently large head circumference and wide set eyes.